Numbness and Tingling: What Your Body Is Trying to Tell You
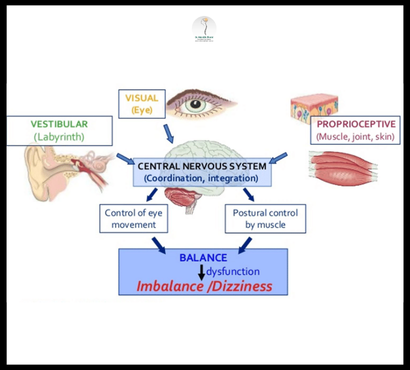
Almost everyone experiences numbness and tingling at some point—whether it’s a foot “falling asleep” after sitting cross-legged, hands tingling after typing for hours, or fingers prickling in cold weather. These sensations may seem trivial, but sometimes they signal something deeper, from nutritional needs to nerve problems or chronic diseases. This guide explores what numbness and tingling really mean, how to distinguish harmless from serious causes, and when to seek medical advice in India’s unique health context. What Are Numbness and Tingling? Numbness means reduced or absent sensation in part of the body. Tingling (also called paresthesia) feels like pins-and-needles, crawling, or electric buzzing under the skin. They commonly affect the hands, feet, arms, legs, fingers, or toes—but can occur in other areas too. Temporary Causes: Everyday Triggers Most occasional episodes are harmless, lasting only a few minutes: Pressure on nerves: Sitting on a leg, lying on an arm, or wearing tight clothing compresses nerves and blood vessels. The sensation vanishes once you change position or move. Cold weather: Blood vessels constrict, reducing sensation, especially in hands and feet. After repetitive use: Typing, writing, or tool use strains nerves and may bring brief tingling. Minor injuries: Bruises or minor sprains can temporarily impair nearby nerves. If symptoms resolve quickly after changing posture or massaging the limb, there’s usually no reason to worry. When Should You Be Concerned? Long-lasting or frequent numbness/tingling, or symptoms that disrupt daily activities, may reveal underlying medical problems: Persistent or increasing symptoms Associated weakness, pain, or muscle loss Loss of coordination, balance, or fine motor skills Symptoms spreading to new areas Difficulty speaking, swallowing, or seeing Bladder or bowel changes Urgent symptoms—such as sudden numbness on one side of the body (possible stroke)—require immediate medical attention. Common Medical Causes Cause Description & Typical Symptoms Diabetes (Peripheral Neuropathy) High blood sugar damages nerves, causing tingling, burning, or numbness in feet/hands; common in India. Vitamin B12 Deficiency Poor diet, vegetarianism, or absorption problems lead to nerve damage—symptoms in legs, arms, mood changes. Carpal Tunnel Syndrome Pressure on wrist nerves causes numbness/tingling in fingers, especially after repetitive activities. Stroke/TIA Sudden loss of sensation, usually one side of body, with speech or vision changes; medical emergency. Thyroid Disease Low thyroid (hypothyroidism) can cause nerve problems, tiredness, cramps, weight gain. Raynaud’s Phenomenon Fingers/toes turn white and numb in response to cold/stress due to poor blood flow; more common in women. Multiple Sclerosis Autoimmune attack on nerves—patches of numbness, tingling, or weakness, vision issues, fatigue. Pinched Nerves/Spine Problems Herniated spine disc or injury compresses nerves—symptoms depend on location (neck, back, limbs). Infection or Inflammatory Disease Shingles, HIV/AIDS, lupus, and other diseases may damage nerves. Chemotherapy/Toxins Medicine or chemicals can cause numbness, tingling, balance issues. Symptoms by Body Part Area Possible Causes Fingers Carpal tunnel, B12 deficiency, diabetes, MS Feet/Toes Diabetes, B12 deficiency, spine issues, Raynaud’s Face Stroke, MS, nerve injury, infection Arms/Legs Spine problems, vitamin/thyroid issues, MS Symptom location helps doctors narrow the diagnosis. Diagnosing the Problem Doctors use a combination of: Detailed symptom history (onset, frequency, triggers) Physical examination (testing sensation, strength, reflexes) Blood tests (diabetes, vitamins, thyroid, kidney function) Nerve conduction studies (detect how quickly nerves send signals) Imaging: MRI, CT scan to check for nerve/spinal cord issues or brain injuries Early diagnosis helps prevent permanent damage and guides correct treatment. Treatment: Root Cause First There’s no universal “cure”—instead, treatment targets the underlying problem: Diabetes: Blood sugar control, medicines, lifestyle change Vitamin deficiency: Supplements (B12, folate), balanced diet Thyroid disease: Medication to restore hormone levels Carpal tunnel: Wrist splints, physiotherapy, sometimes minor surgery Raynaud’s: Keep hands/feet warm, avoid cold, blood vessel medicine if severe Nerve/spine problems: Physical therapy, pain management, surgery in rare cases Infection/inflammation: Medicines tailored to diagnosis Medication-induced: Dose adjustment or switch Prevention Strategies Maintain healthy weight Control diabetes and blood pressure Eat a varied diet (dals, milk, nuts, green vegetables, eggs) Avoid nerve-damaging toxins (alcohol, smoking, excess junk food) Take breaks during repetitive work Practice safe posture and ergonomics Protect hands and feet in cold weather Indian dietary traditions—rich in grains, legumes, and fresh produce—support nerve health. How to Monitor Symptoms Keep a journal of frequency, triggers, duration, and severity. Note any new medicines, recent infections, or stressful events. Report new or worsening changes promptly at your next checkup—timing and pattern provide essential clues. FAQ How do I know if my numbness/tingling is serious? If it’s brief, resolves quickly, and doesn’t recur, it’s likely minor. Persistent, progressive, or sudden-onset symptoms (especially with other deficits) deserve rapid medical attention. Can these symptoms go away by themselves? Temporary episodes due to pressure or posture resolve with movement. Underlying medical causes improve when treated properly but may persist or progress without care. Are blood tests necessary for tingling and numbness? Yes—tests for diabetes, vitamins, thyroid, kidney function, and other conditions are useful. Sometimes nerve studies or scans are added if major nerve or brain disorders are suspected.
Numbness and Tingling: What Your Body Is Trying to Tell You Read More »